There are numerous procedures which form part of a comprehensive eye examination. These can vary from practice to practice and even between practitioners. Some patients may become anxious about what will happen when they get their eyes examined. Knowing what will happen can ease some of this anxiety. Below we will summarize some of the more common procedures you may encounter.
Case History
This is when the Optometrist will ask you about why you are there to have your eyes examined. Are you having any specific issues? Are you having any vision concerns? Are you getting headaches? How long has it been since your last eye examination? They may ask about your general health as some conditions, such as Diabetes may affect your eyes. Some medications can affect your eyes and can have implications if you require any treatment for your eyes. Your family history is important so its helpful if you are familiar with any eye conditions particularly immediate family members may have. They may even ask you about your lifestyle and occupation so they can understand how you use your eyes.
Auto Refraction
This can sometimes be performed as part of a pre-screening process. It involves looking into a machine at a picture like a hot air balloon. By looking at the hot air balloon the accommodative system or focus of the eye is relaxed to improve the accuracy of the results as the hot air balloon replicates a distant object. The machine then determines the curvature of the eye and the refraction of the eye. The refraction is determines whether the light is focussing in front or behind the retina. If light does not focus on the retina eye sight may be blurry and as such spectacles may be required. Auto refraction is generally a really good starting point to determining the refractive error of the eyes. Some other eye conditions such as Cataracts, corneal scars, or Pterygiums can affect the accuracy of the results.

Retinal photo and OCT
This is also generally performed as part of the pre-screening process. The retinal photo takes a photo of the Retina, the back of the eye. It is a great resource and provides a prolonged view of the image rather than having to shine bright lights into the eye. It enables future comparison if things change in the eye. The patient is also able to see the image and understand what the eye professional is explaining.
An OCT (Optical Coherence Tomography) provides a scan through the different layers of the eye. This provides invaluable diagnostic information on the health of the eye. Previously only available to retinal eye specialists, this technology is now widely available to most primary eye health professionals. Some companies may charge a fee to access this technology.

Intraocular Pressure (IOP)
The Intraocular Pressure is a measure of the internal pressure of the eye. There numerous instruments which can be used to measure the IOP. Some are more invasive and are placed on the surface of the eye. Others involve a puff of air onto the surface of the eye. They are all relatively quick and provide a reasonably accurate measurement. IOP is particularly important in regards to the diagnosis and management of Glaucoma.

Retinoscopy
This is performed by the Optometrist and is similar to the auto refraction. A handheld instrument is used to shine a light into one eye of the patient. This light reflects off the retina at the back of the eye. The optometrist will use optical lenses of different power to determine the refraction of the eye. Retinoscopy can be used on all patients, however it is particularly useful when testing children or patients who may have trouble with communication. The Retinoscopy result will usually be used as a starting point for the Subjective Refraction.

Subjective Refraction
Subjective Refraction involves the Optometrist asking the patient which view looks better with different lens options. Often they will ask if the letters on the chart look better with view 1 or view 2. This is usually a refinement of the auto refraction or retinoscopy result and will form your prescription for glasses. The Optometrist aim is to provide clear, comfortable, single vision in the optical device and they will use their clinical judgement to assist with this.

Slit Lamp examination
A slit lamp is a specialized microscope which enables the health professional to view the anterior and posterior segments of the eye. This assists with the diagnosis of pathology by providing a clear magnified image of the eye. The Anterior segment of the eye includes the lids, lashes, cornea, conjunctiva, pupil, iris, and lens. These components of the eye are viewed through the eye piece of the microscope with a thin slit beam of light used to obtain a clear image of the eye. The health professional will be looking for any signs of pathology like sun damage, lumps & bumps, inflammation or redness.

Indirect Ophthalmoscopy (Volk)
To view the back (posterior) of the eye a special lens is used to look through the pupil of the eye and view the retina at the back of the eye. If the pupil is too small, dilating drops may be used to increase the size of the pupil and improve the view of the retina. The special retinal lens is held just in front of the eye by the health professional. This procedure assist with identifying conditions such as Glaucoma, Macula degeneration, Diabetic Retinopathy just to name a few.

Visual Field Test
A visual field test, also known as perimetry, is a diagnostic tool used by eye care professionals to assess the full horizontal and vertical range of what an individual can see in their field of vision. The test helps detect any abnormalities or deficiencies in the peripheral (side) vision, which may be indicative of various eye diseases or neurological conditions.
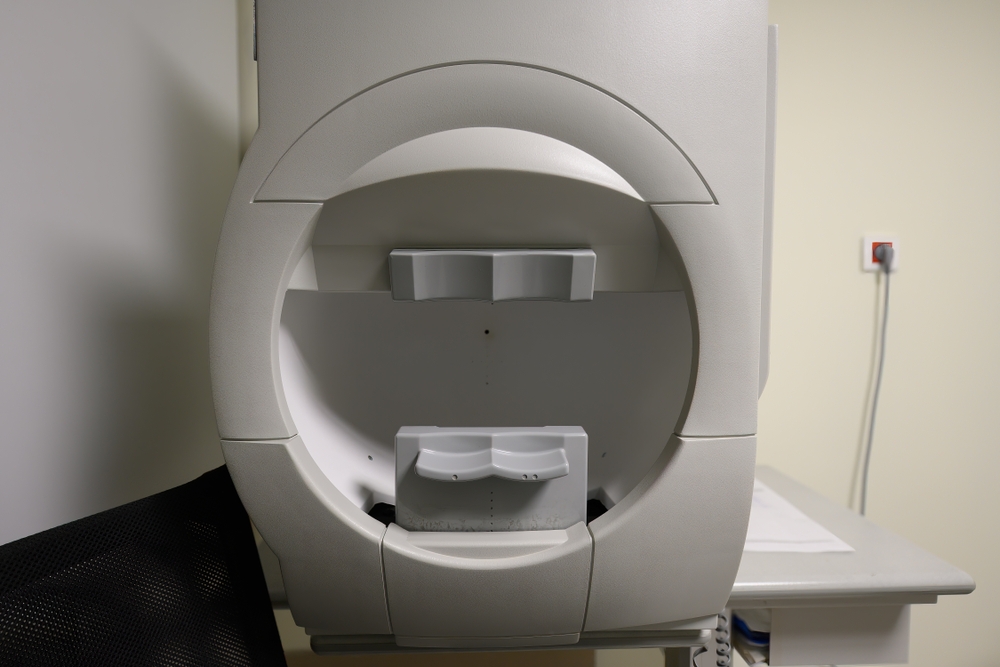
During a visual field test, the person being tested typically sits facing a concave dome or a computerized instrument. New technology in this area is utilizing Virtual Reality headsets to perform Visual field tests. This provides additional comfort to the patient while performing the test. They are asked to focus on a fixed point, while lights or stimuli are presented at various locations within their visual field. The person responds by indicating when they see the stimuli, and the results are then used to create a visual field map.

This test is particularly useful in diagnosing and monitoring conditions such as glaucoma, retinal disorders, optic nerve diseases, and certain neurological disorders. It provides valuable information about the sensitivity of different areas of the visual field, helping eye care professionals assess the health of the entire visual system.
