Diabetes is a chronic metabolic disorder that affects millions of people worldwide. While most individuals are aware of the condition’s impact on blood sugar levels, the effects of diabetes extend far beyond that. One crucial aspect that often goes unnoticed is its detrimental impact on the eyes. In this article, we will explore how diabetes affects the eyes and discuss various eye related complications that individuals with diabetes may encounter.
Diabetic Retinopathy:
Diabetic retinopathy is one of the most common eye conditions associated with diabetes. It occurs when high blood sugar levels damage the blood vessels in the retina, the light-sensitive tissue at the back of the eye. Over time, these blood vessels may leak or become blocked, leading to vision impairment or even blindness if left untreated. Symptoms of diabetic retinopathy include blurred vision, dark spots in the field of vision, and difficulty perceiving colors. Regular eye examinations and managing blood sugar levels are crucial in preventing or delaying the progression of this condition.

Diabetic Macular Edema:
Diabetic macular edema (DME) is a complication of diabetic retinopathy that specifically affects the macula, the central part of the retina responsible for sharp, detailed vision. High blood sugar levels can cause fluid to accumulate in the macula, leading to swelling and distortion of vision. Individuals with DME may experience blurry or distorted vision, difficulty reading, and a decreased ability to recognize faces. Treatment options for DME include laser therapy, intravitreal injections, and medications that reduce fluid buildup.
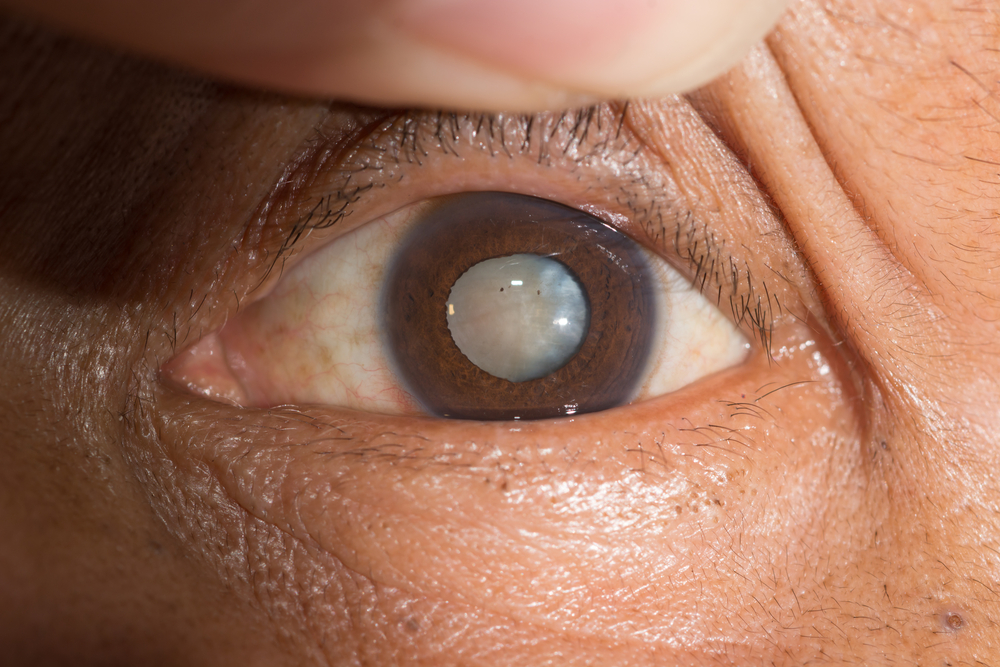
Cataracts:
Cataracts, a common eye condition in the general population, occur more frequently and at an earlier age in individuals with diabetes. A cataract is the clouding of the eye’s natural lens, resulting in blurry or cloudy vision. High blood sugar levels can cause the lens to swell, altering its transparency and leading to the development of cataracts. Cataracts can be surgically removed and replaced with an artificial lens to restore vision. However, it’s important to note that individuals with diabetes may have a higher risk of complications during cataract surgery.
Glaucoma:
People with diabetes are at a higher risk of developing glaucoma, a group of eye diseases that damage the optic nerve and can lead to irreversible vision loss. The exact relationship between diabetes and glaucoma is not yet fully understood, but it is believed that the increased pressure within the eye caused by fluid buildup contributes to optic nerve damage. Regular eye exams, early detection, and treatment are crucial in managing glaucoma. Symptoms may not be noticeable until later stages, making regular screenings even more essential.
Diabetes and Cornea:
The cornea, the clear front surface of the eye, can also be affected by diabetes. Elevated blood sugar levels can lead to changes in the cornea’s structure and function, resulting in conditions such as corneal neuropathy and decreased sensitivity. These changes can cause dryness, blurred vision, and increased susceptibility to infections. Proper management of blood sugar levels and the use of artificial tears or other lubricating eye drops can help alleviate these symptoms.
Prevention and Management:
While diabetes-related eye complications may seem daunting, several measures can be taken to prevent or manage them effectively:
- Regular Eye Examinations: Annual comprehensive eye exams are crucial for individuals with diabetes. These exams allow eye care professionals to detect early signs of any eye-related complications and provide appropriate interventions.
- Blood Sugar Control: Managing blood sugar levels within the target range significantly reduces the risk and progression of diabetic eye diseases. Adhering to a healthy diet, engaging in regular exercise, and taking prescribed medications can help maintain stable blood sugar levels.
